Abstract
Background:
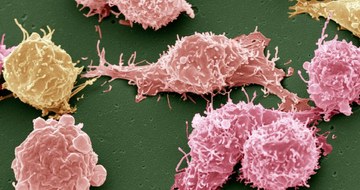
The prognosis of patients with early relapsed or refractory large B-cell lymphoma after the receipt of first-line chemoimmunotherapy is poor.
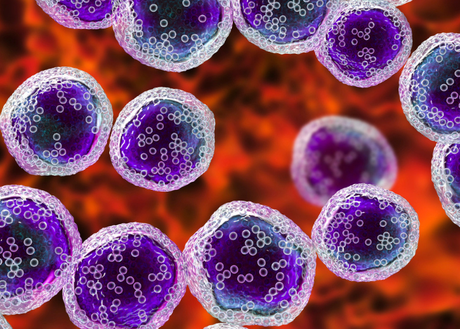
Methods: In this international, phase 3 trial, we randomly assigned, in a 1:1 ratio, patients with large B-cell lymphoma that was refractory to or had relapsed no more than 12 months after first-line chemoimmunotherapy to receive axicabtagene ciloleucel (axi-cel, an autologous anti-CD19 chimeric antigen receptor T-cell therapy) or standard care (two or three cycles of investigator-selected, protocol-defined chemoimmunotherapy, followed by high-dose chemotherapy with autologous stem-cell transplantation in patients with a response to the chemoimmunotherapy). The primary end point was event-free survival according to blinded central review. Key secondary end points were response and overall survival. Safety was also assessed.
Results:
A total of 180 patients were randomly assigned to receive axi-cel and 179 to receive standard care. The primary end-point analysis of event-free survival showed that axi-cel therapy was superior to standard care. At a median follow-up of 24.9 months, the median event-free survival was 8.3 months in the axi-cel group and 2.0 months in the standard-care group, and the 24-month event-free survival was 41% and 16%, respectively (hazard ratio for event or death, 0.40; 95% confidence interval, 0.31 to 0.51; P<0.001). A response occurred in 83% of the patients in the axi-cel group and in 50% of those in the standard-care group (with a complete response in 65% and 32%, respectively). In an interim analysis, the estimated overall survival at 2 years was 61% in the axi-cel group and 52% in the standard-care group. Adverse events of grade 3 or higher occurred in 91% of the patients who received axi-cel and in 83% of those who received standard care. Among patients who received axi-cel, grade 3 or higher cytokine release syndrome occurred in 6% and grade 3 or higher neurologic events in 21%. No deaths related to cytokine release syndrome or neurologic events occurred.
Conclusions:
Axi-cel therapy led to significant improvements, as compared with standard care, in event-free survival and response, with the expected level of high-grade toxic effects. (Funded by Kite; ZUMA-7 ClinicalTrials.gov number, NCT03391466.).