Introduction
Colorectal cancer (CRC) is the fourth most common cancer diagnosed in the United States (US) and second leading cause of cancer death in the US and worldwide.1 CRC incidence has been decreasing over time, with 151,030 new CRC diagnoses and 52,580 CRC-related deaths anticipated in 2022.1 The overall decreased CRC incidence has been largely attributed to routine screening adoption. Screening is especially beneficial in detection of early-stage CRC and may allow for removal of precancerous polyps via colonoscopic polypectomy. The median age at diagnosis is 66, but CRC prevalence has been steadily increasing in the younger population with a reported 51% CRC incidence increase in adults <55 years of age from 1994 – 2014 and an 11% mortality increase from 2005 – 2015.2,3,4 Colon cancer screening is considered the most impactful approach to reduce mortality, though an estimated 46 – 63% of CRC-related deaths may be attributed to missed screening opportunities.5 The observed increase of CRC incidence in younger adults, and results from updated decision modeling data, led multiple organizations to reevaluate average-risk CRC screening recommendations within the last two years.
The initial Cancer Intervention and Surveillance Modeling Network (CISNET) decision models that informed the 2016 US Preventive Services Task Force (USPSTF) guidelines were calibrated based on CRC incidence rates from SEER program registries from 1975 – 1979, a time with limited screening.6 However, in response to the observed CRC incidence increase in patients <55 years old, the CISNET models drafted in 2020 reevaluated the optimal age to initiate screening.6 Modeling evaluated the six screening modalities: 1) colonoscopy, 2) fecal immunochemical testing [FIT], 3) high-sensitivity-guaiac-based fecal occult blood testing [HSgFOBT or FOBT], 4) multitarget stool DNA testing [FIT-DNA]), 5) flexible sigmoidoscopy (SIG), and 6) computed tomographic colonography (CTC). The modeling approach based perceived benefit of screening on the measured number of life-years gained (LYG) from the screening strategy.6 Results showed that decreasing the screening age increased the expected LYG for all screening strategies, and benefits were shown to outweigh potential harm and costs. Notably, these CISNET models assume 100% screening compliance. The model ultimately recommended colonoscopy every 10 years, FIT screening annually, SIG every 5 years, and CTC every 5 years for patients aged 45 – 75 years at average risk of CRC.6 Average risk is defined as individuals without a personal or family history of neoplastic colorectal polyps or CRC, high-risk CRC genetic syndromes, inflammatory bowel disease, cystic fibrosis, and those without clinical features of CRC such as gastrointestinal bleeding, iron deficiency anemia, or abnormal imaging.6
Colorectal Cancer Screening Guidelines
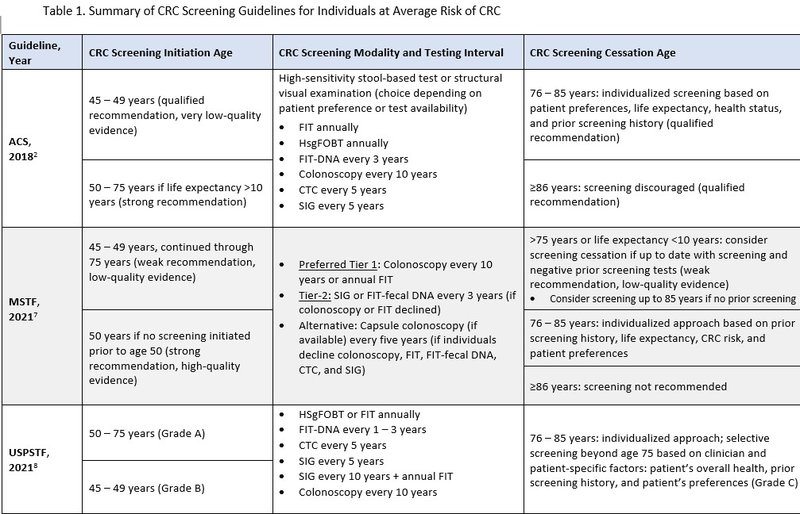
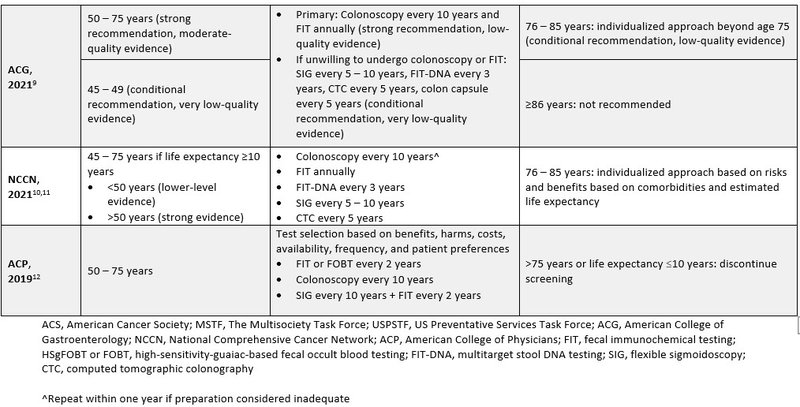
The following organizations recommended lowering the initial screening age from 50 to 45 years for individuals at average risk for CRC: American Cancer Society (ACS), The U.S. Multisociety Task Force (MSTF), USPSTF, American College of Gastroenterology (ACG), and the National Comprehensive Cancer Network (NCCN).2,7-11 The lower screening age aims to reduce the incidence of advanced adenoma, CRC, and mortality from CRC. The strength of recommendation supporting the lowered screening age varied among organizations.2,7-11 The 2019 American College of Physicians guideline held firm with previous recommendations suggesting average risk CRC screening initiation at 50 years.12 Most professional society recommendations suggest screening through 75 years or when life expectancy is less than 10 years, as risks of screening increase with advanced age.7-12 Screening beyond this age should be individualized based on personal screening history, overall health, and patient preference. There were no significant updates for screening modality type for average risk patients, but all positive tests from a non-colonoscopy testing should continue to include timely follow-up with a colonoscopy.2 Table 1 includes a summary of CRC screening guidelines for individuals at average risk of CRC.
Historically, colonoscopy has been regarded as the gold standard for CRC screening. Efficacy data is largely based on cohort studies where design limits the ability to identify confounding factors, though a 2020 systematic review and meta-analyses showed colonoscopy appeared to lower both incidence and mortality of CRC.13-15 However, mortality benefit in randomized trials has only been observed with FOBT and flexible sigmoidoscopy.16,17
NordICC Trial
The Nordic-European Initiative on Colorectal Cancer (NordICC) trial is the first randomized controlled trial (RCT) to evaluate efficacy of CRC screening on risk of CRC development and related death.18 Results of the pre-planned 10-year follow up were published in October 2022. NordICC was a randomized, population-based, pragmatic trial that included patients in Poland, Norway, and Sweden. No screening program was established in this geographic location prior to the start of the trial. Patients were identified via population registries and randomized 1:2 to either receive an invitation to undergo a one-time colonoscopy screening (the invited group, n= 28,220) or no invitation to undergo screening (usual care group, n=56,365).
The co-primary end points were risk of CRC and death from CRC after a median follow-up of 10 to 15 years. The secondary endpoint was all-cause mortality. Results showed the 10-year CRC risk was 0.98% (n=259 cases) in the invited group compared to 1.20% (n=622 cases) in the usual care group, (95% Confidence Interval [CI] 0.70 – 0.93). However, there was no statistically significant difference for the mortality endpoints. The 10-year CRC-related death risk was 0.28% (72 deaths) in the invited group and 0.32% (157 deaths) in the usual-care group, (95% CI 0.64 – 1.16). All-cause mortality was 11.03% in the invited group (3,036 participants) and 11.04% in the usual care group (6,079 participants), (95% CI 0.96 – 1.04). In the invited group, only 42% of patients underwent screening. A pre-specified per-protocol analyses was completed to estimate effect if all patients randomized in the invited group actually underwent screening and showed the risk of death from CRC was 0.15% in the invited group compared to 0.30% in the usual care group, (95% CI 0.27 – 0.77), corresponding to a 50% risk reduction. This also showed 10-year CRC risk was decreased from 1.22% to 0.84%, (95% CI 0.55 – 0.83), corresponding to a 31% risk reduction. The number of individuals needed to invite to undergo screening to prevent one CRC case within 10 years was 455. Adenomas were detected and removed in 30.7% of patients that underwent screening. No new safety concerns related to colonoscopy procedure were reported, as fifteen (0.13%) of participants had polypectomy-related major bleeding; no perforations or screening-related deaths occurred within 30 days after screening.
Results from NordICC do not necessarily indicate lack of benefit from colonoscopy as a screening modality, but rather provide insight regarding efficacy of a new screening program implementation in a population with no previous routine CRC screening. The NordICC investigators recognize there was a lower than anticipated participation in screening and acknowledge longer follow-up is necessary to assess the full effectiveness of colonoscopy screening. They plan to repeat analyses at 15 years. The per-protocol analyses suggest the colonoscopy screening benefit may be under-recognized. The 42% screening rate in the NordICC invited group is lower than the observed 70% CRC screening rate in the US.19 NordICC did not evaluate or stratify for CRC risk factors within the two groups as the population-based design eliminated the ability to distinguish CRC risk differences between the two arms. The observed high rate of CRC detection at screening within the Poland cohort may point to the fact that participants with a perceived high risk of CRC in the invited group tended to undergo screening, an occurrence that would underestimate the effectiveness of colonoscopy within the trial. Additionally, the colonoscopy quality observed in NordICC may be considered suboptimal as 28.6% of endoscopists had an adenoma-detection rate below the recommended 25% benchmark.20 Furthermore, NordICC included patients aged 55 – 64 years of age at randomization, so younger patients that would now be identified as eligible for screening based on recent US screening recommendation updates were not included.
Results of this trial do not change the value of a screening colonoscopy. Benefits of colonoscopy include its prevalence as the only screening modality that both detects and offers removal of any identified cancerous lesions, and there is argument that polyp removal prevents polyp transformation into aggressive adenocarcinoma or other malignant forms. However, colonoscopy is more burdensome than the other screening modalities as the invasive nature requires bowel prep, anesthesia, and a recovery time period following the procedure that may require time off from work. Colonoscopy also requires endoscopist expertise to achieve recommended quality indicators such as recommended benchmarks for cecal intubation and adenoma detection. Other RCTs evaluating colonoscopy compared to less-invasive, more cost-effective strategies are on-going and will provide valuable insight (NCT01239082, NCT00906997).
Cost benefit analysis is necessary when evaluating screening programs and modalities, though an in-depth cost analysis review is beyond the scope of this publication. Insurance companies appear to support screening recommendation updates as multiple reportedly now cover CRC screening starting at 45 years. NordICC results may cause payors to favor less expensive screening modalities such as SIG or the stool-based tests, so we may see a shift in popularity of these modalities. Per an ACS cost analysis model, FIT is considered the most cost-effective modality in CRC screening set to begin at age 45.21
Conclusion
Will colonoscopy remain the gold standard screening tool? Only time will tell. Despite screening update variations, experts will likely agree any CRC screening is better than no screening. However, as evidenced by NordICC, evaluating screening test efficacy is difficult when screening is not performed. As comparative RCTs continue to provide new data, less invasive tests may gain popularity and improve adherence to screening. While ongoing RCTs are comparing CRC screening modalities (NCT01239082, NCT00906997, NCT02078804), future RCTs should aim to include younger participants to better understand impacts of earlier screening and capture any associated mortality benefit. Future analyses evaluating underrepresented populations and corresponding access to screening are also warranted.
References:
- SEER Cancer Stat Facts: Colorectal Cancer. National Cancer Institute. Bethesda, MD. https://seer.cancer.gov/statfacts/html/colorect.html
- Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, Etzioni R, McKenna MT, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018 Jul;68(4):250-281. Epub 2018 May 30. PMID: 29846947.
- Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109(8).
- Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020 May;70(3):145-164. Epub 2020 Mar 5. PMID: 32133645.
- Ladabaum U, Dominitz JA, Kahi C, Schoen RE. Strategies for Colorectal Cancer Screening. Gastroenterology. 2020 Jan;158(2):418-432. doi: 10.1053/j.gastro.2019.06.043. Epub 2019 Aug 5. PMID: 31394083.
- Peterse EFP, Meester RGS, Siegel RL, Chen JC, Dwyer A, Ahnen DJ, Smith RA, Zauber AG, Lansdorp-Vogelaar I. The impact of the rising colorectal cancer incidence in young adults on the optimal age to start screening: Microsimulation analysis I to inform the American Cancer Society colorectal cancer screening guideline. Cancer. 2018 Jul 15;124(14):2964-2973. Epub 2018 May 30. PMID: 29846933.
- Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017 Jul;112(7):1016-1030. Epub 2017 Jun 6. PMID: 28555630.
- US Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, Davis EM, Donahue KE, Doubeni CA, Krist AH, Kubik M, Li L, Ogedegbe G, Owens DK, Pbert L, Silverstein M, Stevermer J, Tseng CW, Wong JB. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021 May 18;325(19):1965-1977. Erratum in: JAMA. 2021 Aug 24;326(8):773. PMID: 34003218.
- Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am J Gastroenterol. 2021 Mar 1;116(3):458-479. doi: 10.14309/ajg.0000000000001122. PMID: 33657038.
- Provenzale D, Ness RM, Llor X, Weiss JM, Abbadessa B, Cooper G, Early DS, Friedman M, Giardiello FM, Glaser K, Gurudu S, Halverson AL, Issaka R, Jain R, Kanth P, Kidambi T, Lazenby AJ, Maguire L, Markowitz AJ, May FP, Mayer RJ, Mehta S, Patel S, Peter S, Stanich PP, Terdiman J, Keller J, Dwyer MA, Ogba N. NCCN Guidelines Insights: Colorectal Cancer Screening, Version 2.2020. J Natl Compr Canc Netw. 2020 Oct 1;18(10):1312-1320. PMID: 33022639.
- National Comprehensive Cancer Network. Colorectal Cancer Screening (Version 3.2022). https://www.nccn.org/login?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
- Qaseem A, Crandall CJ, Mustafa RA, Hicks LA, Wilt TJ; Clinical Guidelines Committee of the American College of Physicians, Forciea MA, Fitterman N, Horwitch CA, Kansagara D, Maroto M, McLean RM, Roa J, Tufte J. Screening for Colorectal Cancer in Asymptomatic Average-Risk Adults: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019 Nov 5;171(9):643-654. Erratum in: Ann Intern Med. 2020 Apr 7;172(7):512. PMID: 31683290.
- Nishihara R, Wu K, Lochhead P, et al: Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 369:1095-105, 2013.
- Doubeni CA, Corley DA, Quinn VP, et al: Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: A large community-based study. https://gut.bmj.com/content/67/2/291
- Zhang J, Chen G, Li Z, Zhang P, Li X, Gan D, Cao X, Du H, Zhang J, Zhang L, Ye Y. Colonoscopic screening is associated with reduced Colorectal Cancer incidence and mortality: a systematic review and meta-analysis. J Cancer. 2020 Aug 15;11(20):5953-5970. PMID: 32922537.
- Mandel JS, Bond JH, Church TR, et al: Reducing mortality from colorectal cancer by screening for fecal occult blood: Minnesota Colon Cancer Control Study. N Engl J Med 328:1365-1371, 1993.
- Holme O, Loberg M, Kalager M, et al: Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: A randomized clinical trial. JAMA 312:606-615, 2014.
- Bretthauer M, Løberg M, Wieszczy P, Kalager M, Emilsson L, Garborg K, Rupinski M, Dekker E, Spaander M, Bugajski M, Holme Ø, Zauber AG, Pilonis ND, Mroz A, Kuipers EJ, Shi J, Hernán MA, Adami HO, Regula J, Hoff G, Kaminski MF; NordICC Study Group. Effect of Colonoscopy Screening on Risks of Colorectal Cancer and Related Death. N Engl J Med. 2022 Oct 27;387(17):1547-1556. Epub 2022 Oct 9. PMID: 36214590.
- QuickStats: Percentage of adults aged 50- 75 years who met colorectal cancer screening recommendations: National Health Interview Survey, United States, 2018. MMWR Morb Wkly Rep 69:314; 2020.
- Bretthauer M, Kaminski MF, Løberg M, Zauber AG, Regula J, Kuipers EJ, Hernán MA, McFadden E, Sunde A, Kalager M, Dekker E, Lansdorp-Vogelaar I, Garborg K, Rupinski M, Spaander MC, Bugajski M, Høie O, Stefansson T, Hoff G, Adami HO; Nordic-European Initiative on Colorectal Cancer (NordICC) Study Group. Population-Based Colonoscopy Screening for Colorectal Cancer: A Randomized Clinical Trial. JAMA Intern Med. 2016 Jul 1;176(7):894-902. PMID: 27214731
- Shaukat A, Levin TR. Author Correction: Current and future colorectal cancer screening strategies. Nat Rev Gastroenterol Hepatol. 2022 Aug;19(8):551. Erratum for: Nat Rev Gastroenterol Hepatol. 2022 Aug;19(8):521-531. PMID: 35787665.